Vulnerable Patients:
Primary Immunodeficiency
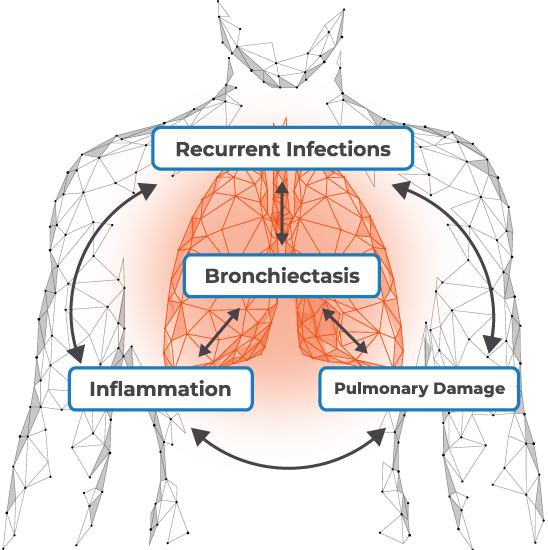
Recurrent infections and other risk factors can lead to a vicious cycle of repeated infections, inflammation, and airway destruction.2
In a long-term study of 473 patients with PID
Despite treatment with immune globulin therapy, recurrent respiratory infections are the most common clinical feature of PID and have the greatest impact on quality of life, including physical and social functioning.2
Failure to recognize and address these high-risk populations can result in long-term respiratory complications, increased hospitalizations, and mortality for patients.2,8
What risk factors suggest this patient needs a change?
History of hypogammaglobulinemia and recurrent respiratory tract infections
Recurrent bacterial and viral infections despite IVIG dose increases and prophylactic antibiotics
History of bronchiectasis
Physical Exam
Presented at the hospital with a fever and respiratory distress
Vital signs on presentation:Hospital Course
Admitted into the hospital and received IV fluids and broad-spectrum antibiotics
- Chest X-ray was consistent with pneumonia of unknown etiology
On day 3, all cultures were NGTD except NP swab, which was positive for PIV.
Labs/Imaging
Chest CT scan revealed interstitial pneumonia with bronchiectasis
PaO2 = 65 mm HgFollow-Up
One week after hospitalization, developed hypotension requiring vasopressors
Immunocompromised patients face a number of clinical challenges associated with RVI, including co-infections, progression to lower respiratory tract infection, and potentially death.
Learn about the advantages and limitations of RVI management strategies in immunocompromised patients.
Cases are hypothetical. Images and descriptions are for illustrative purposes only
COPD, chronic obstructive pulmonary disease; CT, computed tomography; IV, intravenous; IVIG, intravenous immunoglobulin; NGTD, no growth to date NP; nasopharyngeal PID, primary immunodeficiency; PIV, parainfluenza; RVI, respiratory viral infection.
References
1. Jolles S. Clin Exp Immunol. 2014;178(Suppl 1):67-69. 2. Cinetto F, et al. Eur Respir Rev. 2018;27:180019. 3. Llor C, Bjerrum L. Ther Adv Drug Saf. 2014;5(6):229-241. 4. Berger M, et al. Respir Med. 2017;132:181-188. 5. Raje N, Dinakar C. Immunol Allergy Clin North Am. 2015;35(4):599-623. 6. Pagano L, et al. J Antimicrob Chemother. 2011;66(Suppl 1):i5-i14. 7. Resnick ES, et al. Blood. 2012;119(7):1650-1657. 8. Baumann U, et al. Front Immunol. 2018;9:1837.












