-
Physical Exam
Presented at the hospital with a fever and respiratory distress
Vital signs on presentation: -
Hospital Course
Admitted into the hospital and received IV fluids and broad-spectrum antibiotics
- Chest X-ray was consistent with pneumonia of unknown etiology
On day 3, all cultures were NGTD except NP swab, which was positive for PIV.
-
Labs/Imaging
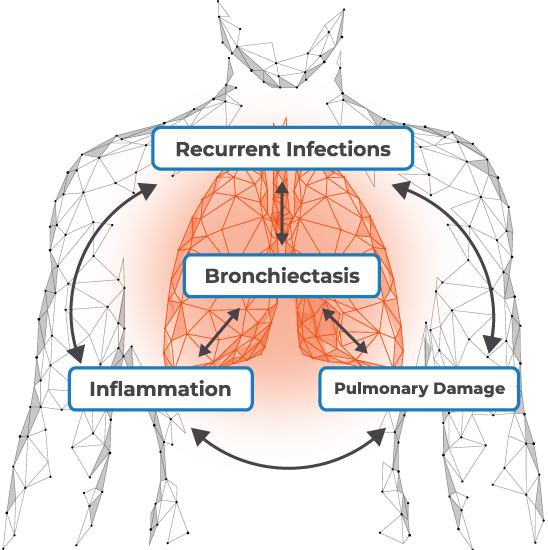
Chest CT scan revealed interstitial pneumonia with bronchiectasis
PaO2 = 65 mm Hg -
Follow-Up
One week after hospitalization, developed hypotension requiring vasopressors